Do Employers Have to Offer COBRA? Compliance Tips & Guidance
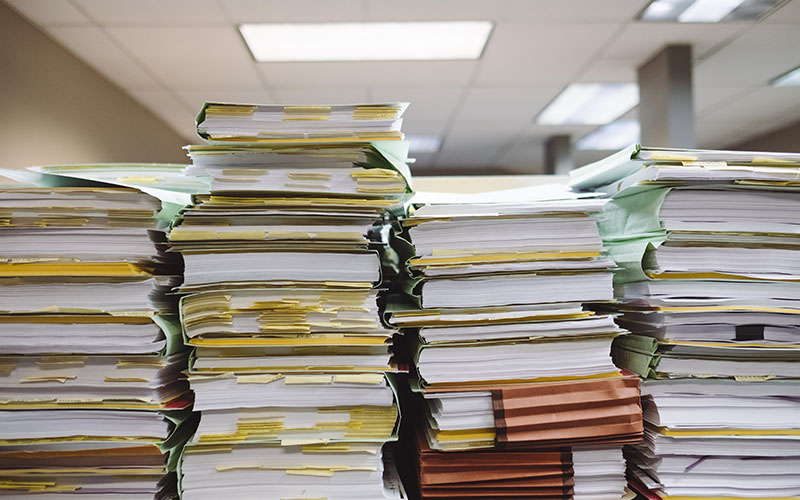
One of the biggest challenges when an employee leaves is making sure you comply with the laws and regulations governing the employee relationship through the very end. While there are a lot of things to consider during this time, we know that COBRA compliance, in particular, is one of the most complex. You may be wondering if you have to offer COBRA and what your responsibilities are as an employer if you do. To help ease your mind, we’ll cover the answers to these questions and more. Let’s get started.
Since it’s essential to get COBRA right or you risk fines or even lawsuits, here, we’ll deconstruct the rules so you know if you need to offer COBRA and what steps you need to take if you do. After reading this, you’ll know what your company needs to do to make sure you stay compliant with COBRA requirements for employers when workers leave your organization.
First off, what is COBRA?
To protect workers from disruptions to their health coverage, the Employee Retirement Income Security Act (ERISA) provides employees the right to Consolidated Omnibus Budget Reconciliation Act (COBRA) continuation coverage.
COBRA gives workers who lose their health benefits (as well as their spouse, former spouse, and dependent children) the ability to continue the coverage provided by their employer for a certain period of time following life changes called qualifying events. These include:
- The death of the employee
- The employee’s loss of a job, unless it was for gross misconduct
- The employee becomes eligible for Medicare
- The employee’s divorce or separation
- A child’s loss of dependent status under the plan
While you may offer other benefits to employees like life insurance, COBRA only covers plans for medical care, including dental and vision care.
Who has to offer COBRA?
Since you’re reading this, you probably want to know, do employers have to offer COBRA? Like a lot of employment laws, the size of your company determines whether you’re covered by the act and need to maintain COBRA compliance. Specifically, COBRA applies to employers with 20 or more employees in the previous year. When determining if COBRA applies to you, it’s important to know that both full- and part-time workers count.
However, even with 20 or more employees, you don’t have to offer COBRA to employees who either weren’t eligible yet for group coverage before they were terminated or those who opted not to participate in your plan.
State Mini-COBRA Laws
While you may not have to offer COBRA coverage because of your size, be aware that in many states, if you have less than 20 employees, you’ll need to provide something called mini-COBRA or state continuation coverage.
The state continuation laws vary in their eligibility rules and coverage terms. So you’ll want to check with your local labor department to find out if there’s a law in your state that affects your company and examine it closely.
Do I Have to Pay for COBRA?
Although you can choose to provide COBRA continuation coverage at a reduced cost or no cost to your employees, you’re not required to pay any part of the premium to maintain COBRA compliance. In fact, you can require your former employees or their dependents to pay the entire premium. However, the amount they pay can’t be more than the full cost of coverage plus a two percent administrative fee. Plans also must give 45 days after an individual elects coverage before requiring them to pay a premium.
Because of the higher costs of COBRA coverage, not all employees will opt to continue their group benefits. Instead, they may choose alternatives like enrolling in their spouse’s plan or in an individual plan with an insurance provider they find in the marketplace.
What are the COBRA requirements for employers to maintain compliance?
If you have to offer COBRA coverage, there are five steps you need to follow to be in compliance with COBRA requirements for employers:
Distribute Proper Notices
When it comes to COBRA compliance, communication is key. There are several notices you need to be aware of that explain COBRA rights. These are provided by the health plan administrator, which may be you.
One is the qualifying event notice, which requires notifying the health plan when an employee is eligible for COBRA. As an employer, you’re only required to notify your plan if you’ve terminated or reduced the hours of an employee, the employee passed away, or they became eligible for Medicare. Otherwise, for example, in the case of divorce, it is up to the employee or qualified beneficiary to notify the plan.
After learning of a qualifying event, your health plan has 14 days to give beneficiaries an election notice that explains how they opt into coverage.
Health plans also need to provide the employee or spouse covered under the plan a COBRA general notice within the first 90 days of coverage. The Department of Labor has a model notice. You can also include this general notice in your Summary Plan Description as long as it’s provided in the timeframe required.
Provide an Election Period
Health plans will have to give qualified beneficiaries a certain amount of time to decide if they’re going to opt into continuation coverage. This time period needs to be at least 60 days from the date of the qualifying event or election notice was provided – whichever is later.
Offer the Same Benefits
To keep up with COBRA compliance for your organization, it’s essential that the continuation coverage offered is the exact same coverage as what’s currently available under the plan to other similar employees. That means beneficiaries need to have the same benefits, choices, and services. Likewise, employees are subject to the same rules for things like co-pays.
Maintain Coverage for a Certain Period
Depending on what triggered COBRA coverage, you’ll either need to offer continuation coverage for 18 or 36 months. If you terminate an employee, they’re eligible for 18 months of coverage unless they became eligible for Medicare less than 18 months before you let them go. In this case, their spouse and dependents are eligible for up to 36 months of coverage. For all other qualifying events, beneficiaries must receive 36 months of coverage.
Let Employees Know if Coverage Ends Early
While there are certain minimum limits for maintaining COBRA coverage, a group plan can terminate continuation coverage early for certain reasons, like if an employee fails to pay the premiums. In these cases, the plan has to provide qualified beneficiaries with an early termination notice.
What are the Fees for not maintaining COBRA compliance?
Like violations of other employment laws, if you fail to follow the COBRA rules, the costs can quickly add up. For example, if you don’t meet the notice requirements, you could be fined $110 per day per qualified beneficiary by the Department of Labor. Plus, the IRS can also impose an excise tax for violations.
Stay ahead of COBRA Compliance With Proper Administration
As you can see, COBRA rules and requirements can be complicated, but the bottom line is that, in most cases, you’ll need to provide either COBRA or mini-COBRA coverage. To mitigate your risk of non-compliance and costly penalties, it’s important to understand what’s required of you to maintain COBRA compliance and review your practices. For some companies without the resources or expertise in-house to manage COBRA administration, it makes more sense to outsource the task to a third party administrator (TPA). If that sounds like you, learn the factors to consider when selecting a COBRA administrator. As you evaluate your options, learn about the COBRA administration services Complete Payroll Solutions offers to see if we may be a good fit for your organization.
This blog was originally published in September of 2020 and was updated in July of 2023 for accuracy and comprehensiveness.
in
 Benefits
,
COBRA
,
Health Benefits
Benefits
,
COBRA
,
Health Benefits